Cultural sensitivity in mental healthcare is crucial for effective superior depression therapy. By recognizing and respecting diverse backgrounds, therapists can tailor approaches, build trust, and empower patients through culturally relevant practices like mindfulness or storytelling. Challenges include lack of cultural awareness among practitioners due to insufficient training, which can lead to miscommunications and hinder treatment. Mental healthcare providers play a vital role in creating safe spaces, actively listening to patients' narratives, and incorporating personalized self-care routines based on cultural contexts, ultimately improving engagement and outcomes while respecting diverse perspectives.
Cultural sensitivity is an essential aspect of mental healthcare, ensuring effective and compassionate patient care. This article explores the critical concept of cultural sensitivity in psychiatric practice, highlighting its significance in understanding diverse patient experiences. We delve into the challenges faced by healthcare providers in delivering culturally competent care and offer strategies to enhance depression therapy tailored to individual cultural backgrounds. By embracing cultural awareness, mental health professionals can significantly improve patient outcomes and satisfaction.
- Understanding Cultural Sensitivity in Mental Healthcare
- Challenges and Barriers to Providing Culturally Competent Care
- Strategies for Delivering Superior Depression Therapy Through a Cultural Lens
Understanding Cultural Sensitivity in Mental Healthcare

Cultural sensitivity in mental healthcare is a critical aspect that often determines the effectiveness and accessibility of treatment. It involves recognizing and appreciating the diverse cultural backgrounds, beliefs, and practices of patients, and tailoring therapeutic approaches accordingly. Understanding this concept is essential for providing superior depression therapy, as cultural factors can significantly influence how individuals experience and express mental health challenges. For instance, what constitutes appropriate communication or disclosure varies across cultures, which directly impacts the patient-therapist relationship and treatment outcomes.
By embracing cultural sensitivity, mental healthcare practitioners can offer more inclusive and effective support. This might involve integrating practices like mindfulness meditation or exploring mind over matter principles that resonate with different cultural perspectives. For example, in some communities, sharing personal experiences openly may be less common, so therapists could adapt by employing non-verbal communication techniques or using storytelling as a therapeutic tool to build trust and encourage participation. Such adaptations not only enhance depression prevention efforts but also foster an environment where patients feel understood and empowered to engage in their healing journey.
Challenges and Barriers to Providing Culturally Competent Care

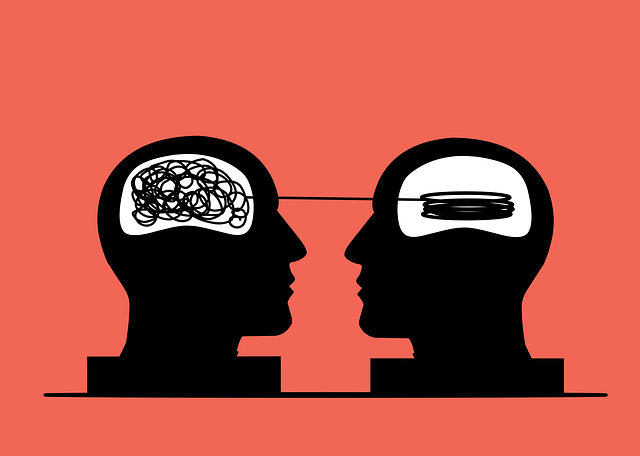
Providing culturally competent care presents unique challenges in mental healthcare. One significant barrier is the lack of cultural awareness among practitioners, often stemming from inadequate training and education on diverse ethnic, racial, and cultural backgrounds. This gap can lead to miscommunications, stereotypes, and even discrimination, hindering effective treatment for patients from various communities. For instance, certain cultural beliefs and practices may influence how individuals express distress or seek help, requiring tailored approaches for superior depression therapy.
Another challenge lies in the intersection of cultural differences with clinical practices, such as burnout prevention strategies for healthcare providers. The diverse patient population demands a wide array of therapeutic methods, including those focusing on mood management. Healthcare professionals must be adept at adapting their techniques to respect and honor patients’ cultural contexts while ensuring effective treatment outcomes. Incorporating culturally sensitive practices not only enhances patient satisfaction but also contributes to reducing disparities in mental healthcare services.
Strategies for Delivering Superior Depression Therapy Through a Cultural Lens

In providing superior depression therapy, mental healthcare practitioners must embrace cultural sensitivity to ensure effective treatment. Understanding a patient’s cultural background is essential as it shapes their beliefs, values, and coping mechanisms related to mental health. By integrating cultural competency into therapy sessions, healthcare providers can create a safe and supportive environment. This involves actively listening to patients’ narratives, respecting their traditional practices, and incorporating self-care routines tailored to their cultural preferences. For instance, encouraging mindfulness meditation or yoga as part of a patient’s self-care practice may resonate deeply with individuals from cultures emphasizing spiritual well-being.
Cultural sensitivity allows therapists to adapt their strategies for superior depression therapy. This might include using culturally relevant therapeutic approaches, such as incorporating family involvement in treatment plans (a common preference in many communities) or teaching stress-reduction techniques that align with a patient’s cultural self-care practices. By considering these factors, mental health professionals can offer personalized care, fostering better engagement and positive outcomes in treating depression while respecting diverse cultural perspectives.
Cultural sensitivity is an indispensable aspect of mental healthcare practice, enabling professionals to deliver superior depression therapy tailored to each individual’s unique cultural background. By understanding and addressing cultural barriers, we can create inclusive environments that foster trust and improve patient outcomes. Embracing diverse perspectives and implementing culturally competent strategies ensures that everyone receives respectful, effective care, ultimately enriching the field of mental health support.